Antibiotic sensitivity-test and result
Antibiotic sensitivity-test and result
Antibiotic sensitivity test
Antibiotic resistance
is understood as the power of bacterium to resist antibiotics because of presence of resistance factor in its genetic material. This factor is also present usually inherited or it may be acquired through horizontal chromosomal mutation events like conjugation, transformation, and transduction. It happens by inactivation of the porin channel, modification of antibiotic targets, and neutralizing antibiotic effectivity through enzymatic action. Therefore changes in bacterium are important to understand the resistance mechanism
Susceptibility test
is used to see that antibiotics can inhibit the expansion of the bacterium or fungi causing a particular infection. The results from this test can facilitate a health care professional confirm that medicine are possible to be the best in treating somebody's infection
Some infections could need testing as a result of the bacterium or fungi isolated from an infection site are identified to own unpredictable susceptibility to the drugs usually used to treat them. This bacteria like staphylococci ("staph") and Pseudomonas aeruginosa
Sometimes there is also more than one kind of microorganism isolated from an infected site, like a wound infection. susceptibility testing is also used to confirm that antibiotic or antibiotic mixtures are going to be best in treating all the various varieties of bacteria causing the infection
Test purpose
To guide the practitioner in choosing the most effective antibiotic agent for a patient
To management the utilization of inappropriate antibiotics in clinical observe
To accumulate epidemiological data on the resistance of microorganisms of public health importance at intervals the community
Type
Qualitative
For the testing of isolates from “healthy” people with intact immune defenses
For less serious infections like uncomplicated urinary tract infections
Quantitative
In the treatment of significant infections like endocarditis or osteomyelitis
For infections in risky patient groups like immunocompromised patients (e.g.. transplant patients)
Antibiotic Sensitivity Tests
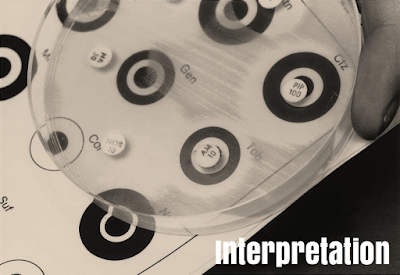
Disk Diffusion Method
Principle
A paper disk with an outlined quantity of antibiotic is used to get a dynamically changing gradient of antibiotic concentrations within the agar within the locality of the disk
The antibiotic contained in a reservoir is allowed to diffuse out into the medium and act during a plate freshly seeded with the test organisms
The disk is put to the surface of an agar plate inoculated with the test bacteria
The antibiotic diffuses out of the disk to make the gradient
The test organism starts to divide and grow and progresses toward a crucial mass of cells
Inhibition zone edge is made at the crucial time wherever a selected concentration of the antibiotic is simply ready to inhibit the organism before it reaches an overwhelming cell mass or crucial mass
Mueller-Hinton Agar
Medium containing beef infusion, peptone, and starch
Used primarily for the disk-diffusion technique
Mueller-Hinton agar is taken into account the most effective for routine susceptibility testing of nonfastidious bacterium
Why
It shows acceptable batch-to-batch reliability for susceptibility testing
It is low in some antibiotics like trimethoprim, sulfonamides, and tetracycline inhibitors
It provides satisfactory growth of most nonfastidious pathogens
A massive body of information and skill has been collected regarding status tests performed with this medium
Antibiotic Disks
Any commercially offered discs with the correct diameter and efficiency are often used
On removal from the refrigerator, the containers ought to be left at room temperature for about one hour to permit the temperature to equilibrate
Measurement of diameter
Using a ruler
under the surface of the plate which contain transparent medium
Using a pair of calipers
on the plate which contain opaque medium
Using automatic zone readers
BIOMIC
Aura
Protozone
Result interpretation
Susceptible,When the edge of the inhibition zone present outside the black circle
Resistant, When there's no zone, or once it lies at intervals the white circle
Intermediate, When the edge of the inhibition zone lies on
the black circle
Using a ruler
The diameter of inhibition zone is usually measured by using a ruler or a pair of calipers
This diameter is interpreted per the critical diameters
Factors influencing size of zone
Inoculum density
Too light substance, Inhibition zones are going to be larger even if the sensitivity of the organism is unchanged. Relatively resistant strains is also incorrectly reported as susceptible
Too significant heavy, Inhibition zones are going to be smaller. Relatively susceptible strains could then be incorrectly reported as resistant
Temperature of incubation
If the temperature is lowered , the time needed for effective growth is extended and bigger zones result
Potency of antibiotic disks
If the effectivity of the drug becomes low due to deterioration throughout storage, the inhibition zone can show a corresponding decrease in size
Dilution ways
Used to see the lowest concentration of antibiotic to inhibit or kill the organism
occurred by dilution of antibiotic in agar or broth media
Minimum inhibitory concentration
The lowest concentration of drug that inhibits the expansion of the bacterium isolated from the patient
The MIC is detected by inoculating the organism isolated from the infected person into a series of tubes or cups which contain progressive dilutions of the drug
Minimum bactericidal concentration
The lowest concentration of drug that kills the microorganism isolated from the patient
E-Test
Epsilometer test
Quantitative technique of antibiotic sensitivity testing
Applies each dilution of antibiotic and diffusion of antibiotic into the medium
Combines the principles of disk diffusion and agar dilution ways
A predefined stable antibiotic gradient is present on a thin inert carrier strip
Using innovative dry chemistry technology
E-Test is used to see the on-scale Minimum inhibitory Concentration (MIC)
E-Test Uses
Determining the MIC of fastidious, slow-growing or nutritionally deficient micro-organisms, or for a particular kind of patient or infection
:Detecting
–Glycopeptide-resistant Enterococci (GRE)
–Glycopeptide-intermediate S. aureus (GISA)
–Resistant mycobacterium tuberculosis
–Extended spectrum beta lactamases (ESBL)
Detecting low levels of resistance
Testing an antibiotic not performed in routine use or a replacement, recently introduced antibiotic agent
Advantages
Simple
Accurate
Reliable