Is the complement system innate or adaptive immunity?
What activates the complement system? And how does complement cause inflammation?
Innate immune system
The two main immunity strategies found in vertebrates are the innate immune system and the adaptive immune system.
The major functions of the vertebrate innate immune system include:
- calling immune cells to sites of infection by the production of chemical factors, including specialized chemical mediators called cytokines
- Activation of the complement system to identify activated cells and bacteria and promote clearance of antibody complexes or dead cells
- It uses specialized white blood cells to identify and remove the foreign substances present in tissues, organs, blood, and lymph.
- Activation of the acquired immune system through a process called antigen presentation
- has a vital role as a physical and chemical barrier to infectious agents; through physical measures such as skin and chemical measures such as clotting factors in blood, which are released following injury that breaks through the first-line physical barrier (not to be confused with a second-line physical or chemical barrier, like the blood-brain barrier, that protects the extremely vital and highly sensitive nervous system from pathogens that have already gained access to the host's body).
Inflammation
It is a type of response from body tissue to harmful stimuli, such as pathogens, irritants, or damaged cells. This is a protective response that includes immune cells, blood vessels, and molecular mediators. The function of inflammation is to release the first cause of cell injury, clear necrotic cells and tissues damaged by the original insult and the inflammatory process, and start tissue repair.
Signs of inflammation
There are five signs of inflammation.
- heat
- pain
- redness
- swelling
- loss of function
Inflammation is a general response, so it is considered a mechanism of innate immunity by comparison to adaptive immunity, which is specific for each type of pathogen. Small inflammation could lead to progressive tissue damage by the harmful stimulus (e.g., bacteria) and affect the survival of the organism. In contrast, chronic inflammation is related to different diseases, like hay fever and periodontal disease.
Classification of inflammation
It can be classified as either acute or chronic. Acute inflammation is the body's first response to harmful stimuli and is caused by the increased movement of plasma and leukocytes (especially granulocytes) from the blood into the injured tissues. A series of biochemical events occur and mature the inflammatory response, including the local vascular system, the immune system, and various cells within the injured tissue. Long-term inflammation, called chronic inflammation, leads to a progressive shift in the kind of cells present at the site of inflammation, like mononuclear characterized by simultaneous damage and healing of the tissue from the inflammatory process.
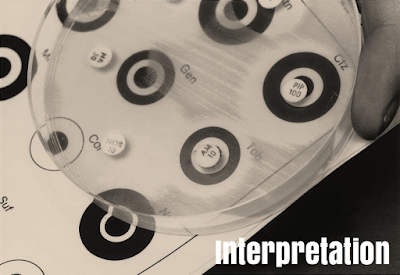
The complement system (complement cascade)
is known as a part of the immune system's heat-labile component in normal plasma that stimulates the ability of antibodies and phagocytic cells to clear microbes and destroy cells from an organism, evoke inflammation, and attack the pathogen's cell membrane. It is part of the innate immune system, which is not adaptable and does not change during an individual's life. The complement system can, however, be brought into action by antibodies that are generated by the adaptive immune system.
The complement system is composed of a number of small proteins that are created by the liver and circulate in the blood as inactive precursors. When stimulated by one of several types of triggers, proteases in the system split specific proteins to release cytokines and start an amplifying cascade of further cleavages. The final result of this complement activation cascade is stimulation of phagocytic cells to clear foreign and damaged material, inflammation to pull additional phagocytes, and activation of the cell-killing membrane attack complex. More than 30 proteins and protein fragments make up the complement system, including serum proteins and cell membrane receptors.
The components of the complement system (proteins and glycoproteins) are synthesized by hepatocytes. But significant amounts are also created by blood monocytes, tissue macrophages, and epithelial cells of the genitourinary system and digestive system. The three pathways of stimulation all generate homologous but different types of protease C3-convertase.
There are three pathways by which complement can be stimulated on the surface of a pathogen. These three pathways depend on various molecules for their start, but they converge to start the same set of effector molecules. First, it forms large numbers of stimulated complement proteins that bind covalently to pathogens, opsonizing them for phagocyte engulfment with complement receptors. Second, the small fragments of some complement proteins work as chemoattractants to call more phagocytes to the site of complement activation and also to stimulate these phagocytes. Third, the final complement components destruct certain bacteria by creating pores in the bacterial membrane.
The classical complement pathway typically needs antigen-antibody complexes for activation, whereas the alternative pathway can be stimulated by spontaneous complement component 3 (C3) hydrolysis, pathogens, foreign material, or damaged cells. The mannose-binding lectin pathway can be stimulated by C3 hydrolysis or antigens without antibodies (non-specific immune response). In all types of complement pathways, C3-convertase cleaves and activates component C3, creating C3a and C3b and causing a cascade of further cleavage and stimulation events. C3b binds to the surface of pathogens, leading to more internalization by phagocytic cells through opsonization.